Efficacy & Safety
Resources

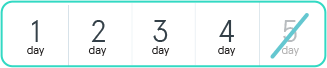
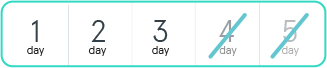
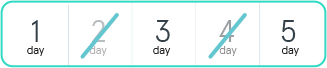
| Week 1 | One tablet once daily for 5 days | 2 days rest |
|---|---|---|
| Week 2 | Rest | |
| Week 3 | Rest | |
| Week 4 | Rest | |

Fixed-dose combination tablet containing decitabine (35 mg) and cedazuridine (100 mg)
Tablet shown is not actual size. Actual tablet size is 7.94 mm x 14.29 mm.


In patients who received INQOVI:
The most frequent cause of dose reduction or interruption was myelosuppression (thrombocytopenia, neutropenia, anemia, and febrile neutropenia).


Delay the next cycle if absolute neutrophil count (ANC) is <1000/μL and platelets are <50,000/μL in the absence of active disease. Monitor complete blood cell counts until ANC is ≥1000/μL and platelets are ≥50,000/μL.
If hematologic recovery does not occur within 2 weeks of achieving remission:
Delay
Reduce
Maintain or increase dose
Delay the next cycle for these nonhematologic adverse reactions and resume at the same or reduced dose once resolved:
1st dose reduction
Dosage:
2nd dose reduction
Dosage:
3rd dose reduction
Dosage:
*Myelosuppression includes thrombocytopenia, neutropenia, anemia, and febrile neutropenia.
If vomiting occurs following dosing:

Within 12 hours of the time it is usually taken:
INQOVI tablets can be substituted for IV decitabine, but not within a cycle.
A response to INQOVI tablets may not be immediate. A complete or partial response may take longer than 4 cycles.
Antiemetics (prior to each dose), growth factors, and anti-infective therapies can be administered for treatment or prophylaxis as appropriate.
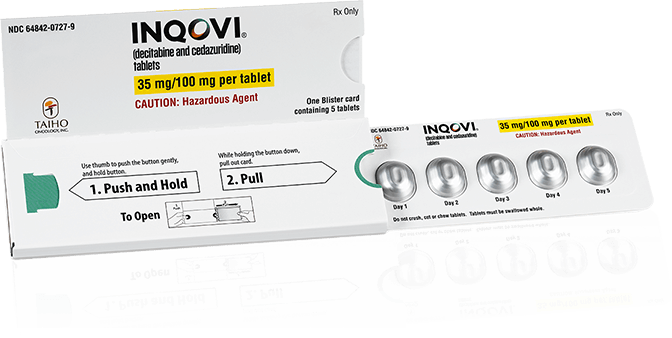
Easy-to-use blister pack
DosePak is 7.35 in x 2.45 in.
HMA=hypomethylating agent.
References: 1. INQOVI [package insert]. Princeton, NJ: Taiho Oncology, Inc.; 2022. 2. Kim N, Norsworthy KJ, Subramaniam S, et al. FDA approval summary: decitabine and cedazuridine tablets for myelodysplastic syndromes. Clin Cancer Res. 2022;28(16):3411-3416.
Efficacy & Safety
Resources